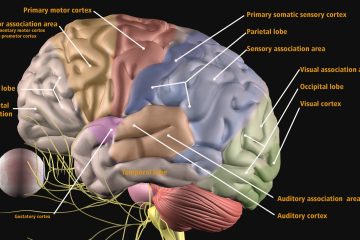
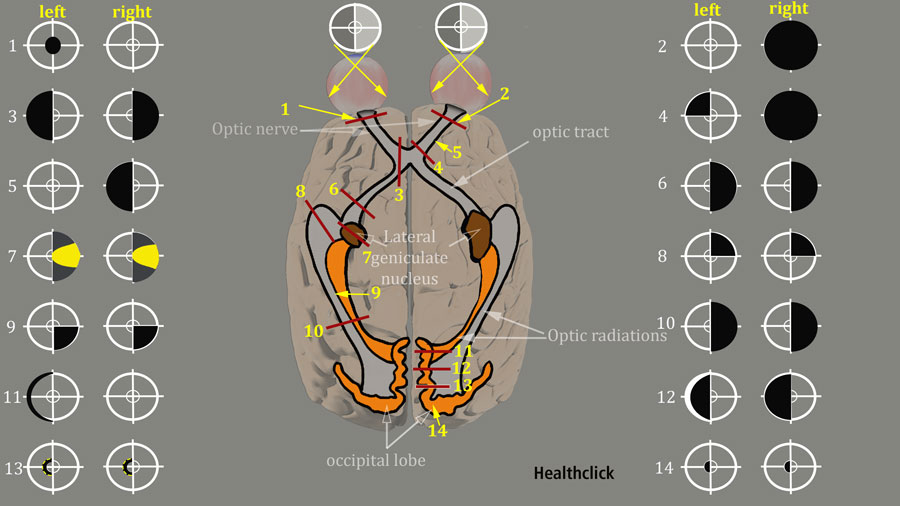
With an occipital stroke, there is the potential for a lot of visual changes in your patient. Your occipital lobes are where you interpret vision. Your retinas are where the image goes back through the optic chiasm and then it is processed in your occipital lobe to give you an idea about what it is that you are actually seeing and how to interpret that. You look at form, motion, and color. If this stroke is severe enough, or you have bilateral involvement you can have cortical blindness from occipital strokes. This is a very difficult thing for people to adjust to because they can see some things, but it is not consistent. These individuals are at high risk for falls because they are not able to see things well. This Stroke Rehab and Visual Impairment Continuing Education Course will help you identify visual impairments associated with a stroke and techniques top address these deficiencies.
As an OT, there are some different batteries you can use to assess vision. Typically I observe first in a normal environment to see if they can do other things:
- Can you see that I am over here? Are they aware that I am over here?
- Can their eyes move in this direction?
- Are they blinking more, or are they squinting?
- Are they trying to cover one eye?
I use the cues that the person’s giving me and, of course, ask the team for support. Ask the family member to request a low vision consult or go straight to the physician and ask them to make a referral for an optometrist or ophthalmologist to diagnose the actual visual deficits.
Even without a formal diagnosis, you need to observe the problems and help them adapt to the environment. Create a perfect balance to challenge them but also make them successful at times. Then at times, set them up for failure and then teach them why they failed. The next time will be a little easier, so they don’t fail, and you can build on that.
I think the main thing for vision is to understand the environment and the specific challenge of that patient and set them up overall for a positive experience so that they can learn with their visual deficits can remember how to build upon that.
There is a substantial amount of evidence that patients can be supported to compensate and adapt to visual field loss following stroke using a range of strategies and methods. However, this systematic review highlights the fact that many unanswered questions in the area of adaptation to visual field loss remain.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6086007/
A huge part is getting that genuine professional opinion and diagnosis from an optometrist or an ophthalmologist.
When with the patient, observe if they are turning their head or if their eyes move, or if they have a genuine lack of awareness. Are their deficits related to an auditory deficit as well or a lack of sensation awareness? Heightened sensitivity to other areas can also affect vision and can cause other problems.
Stroke Rehab and Visual Impairment Continuing Education
Overall, I look at what the patient is doing in an environment that most of us would typically respond to in a specific way. If they react differently, then I take that information, and I will share that with the team or the family and say, “Hey, this is what I am seeing. Do you see the same thing? They are not turning to the left, or they can see me if I am here, but if I move over a few inches, and they can not see me.” I’ am not great at saying, “Hey, I think it’s this specific label,” but I am better at saying, “I think this is where they can see me. This is how we improve that, and let’s build on that.”
Looking for more Stroke Rehab related Continuing Education? Check out our new, all access, online subscription for PT, PTA, OT and AT
New – PT, PTA and OT Continuing Education – All Access Subscription – $189.
References
The video in this blog is referenced from the stroke rehab continuing education course, Stroke – Understanding Etiology and Developing Evidence-Based Pathways to Achieve Functional Outcomes. This online course is included in our all-access annual subscription along with these other stroke related continuing education courses:
- Stroke: Achieving Functional Movement in the Home Bound Patient
- Restoring Functional Gait
- Applying the Principles and Philosophy of PNF to Enhance Gait
- Stroke and The Limbic System
Elizabeth L Saionz, Duje Tadin, Michael D Melnick, Krystel R Huxlin, Functional preservation and enhanced capacity for visual restoration in subacute occipital stroke, Brain, Volume 143, Issue 6, June 2020, Pages 1857–1872, https://doi.org/10.1093/brain/awaa128
Amedi A, Merabet LB, Bermpohl F, Pascual-Leone A. The Occipital Cortex in the Blind: Lessons About Plasticity and Vision. Current Directions in Psychological Science. 2005;14(6):306-311. doi:10.1111/j.0963-7214.2005.00387.x