This week’s series focuses on Cancer Rehab Continuing Education Course material specifically microvascular breast reconstruction. The course Maximizing Post-Surgical Outcomes in Cancer Rehabilitation presents several reconstructive surgical procedures for cancer patients. Today’s topic is reconstruction surgery.
When Does Reconstruction Begin?
Usually, reconstruction starts at the time of a mastectomy; you can even do autologous tissue at the time of mastectomy. This is dependent on the need for radiation treatment and also on the wishes of the patient. Most individuals get some form of tissue expander reconstruction, a temporary spacer placed in the breast. There are also more advanced techniques like implants at the time of mastectomy.
Microvascular Breast Reconstruction
In this cancer rehab course, Dr. Stanwix discusses several types of reconstruction. Today the focus is on the procedure for microvascular breast reconstruction.
What is Microvascular Breast Reconstruction Surgery?
Microvascular breast reconstruction involves removing tissue from one body area, completely disconnecting it, and then reconnecting the little vessels to remake a breast. This procedure follows a mastectomy and is also for breast cancer patients or patients who have this prophylactically done for a BRCA gene mutation. This can be done as a nipple-sparing process where the nipple can be saved or as a skin-sparing process where the rest of the breast skin is saved. Now by taking tissue from one area of the body and transferring it to the other area of the breast, you’ll be able to recreate a breast in the most natural, supple way and recreate like with like, meaning you’re able to create a breast out of tissue that is basically just skin and fat again.
Benefits of Microvascular Reconstruction Surgery
The best part of the surgery is that it uses your own body’s tissue and lasts forever, and it’s also a very low-risk procedure in terms of complications from the other area you’re taking the tissue from. Mostly, or about ninety percent of the time, I take the tissue from the belly. I’m doing a tummy tuck procedure, making an incision low in the bikini line, and then taking that tissue and recreating a new breast.
“However, refinements in microsurgical techniques and improved examination devices may lead to the establishment of standard surgical treatment for lymphedema.“
Article Citation
What is Involved?
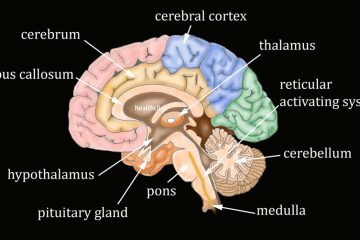
To do the surgery, I take the tummy tuck tissue, just the skin, and the fat, and release it from the underlying muscle. I have to part the muscle to the side to find the little vessels there. Now, these little vessels are just slightly bigger than maybe the size of a small pencil. These small pencil vessels go through the muscle, and I tease the muscles away. I save the hard part that covers the muscle called the fascia. I save the nerve, so you have your strength back. I don’t take the muscle. I’m able to get through the muscle to find the area of the vessel that comes down from the groin, and I completely cut that vessel, take it off this area of the body, and then reconnect it up into the chest. The chest has small vessels called the internal mammaries, which we may use. Sometimes we use the thoracodorsalis, veins, and arteries connecting to your latissimus muscle. I disconnect those vessels and then reconnect the vessels from the groin up to the vessels in the chest to remake that new breast tissue because this procedure involves using a microscope and a suture that is finer than a human hair.
Learn more about Cancer Rehab Education Courses in our All Access Continuing Education Subscription
The Healthclick All Access Online Series in our new All Access Annual Subscription contains a variety of upper extremity orthopedic courses to Improve function. Check out some other courses within the orthopedic series:
The Fundamentals of Lymphedema Treatment
The Physiological Impact of Chronic Pain
Myofascial Release for the Aging Population
Maximizing Post Surgical Outcomes in Cancer Rehabilitation
References
- Brahma, Bayu, and Takumi Yamamoto. “Breast cancer treatment-related lymphedema (BCRL): An overview of the literature and updates in microsurgery reconstructions.” European Journal of Surgical Oncology 45.7 (2019): 1138-1145.
- Chocron, Yehuda, et al. “Axilla versus Wrist as the Recipient Site in Vascularized Lymph Node Transfer for Breast Cancer-Related Lymphedema: A Systematic Review and Meta-Analysis.” Journal of Reconstructive Microsurgery (2021).
- Panchal, Hina, and Evan Matros. “Current trends in post-mastectomy breast reconstruction.” Plastic and reconstructive surgery 140.5 (2017): 7S.
- Suami, Hiroo M.D., Ph.D.; Chang, David W. M.D.. Overview of Surgical Treatments for Breast Cancer–Related Lymphedema. Plastic and Reconstructive Surgery: December 2010 – Volume 126 – Issue 6 – p 1853-1863 doi: 10.1097/PRS.0b013e3181f44658