According to the CDC, there are currently over 36 million falls and 3 million emergency room visits per year. The Balance and Fall Prevention Continuing Education Course, Evidence-Based Outcome Tools for Treating Balance Dysfunction, provides the clinician with evidence-based validity for the tools and techniques utilized to evaluate and treat the imbalanced patient.
This Balance and Fall Prevention Continuing Education Course provides in-depth evaluation and treatment techniques to improve balance and prevent falls. The information below is from an expert from the comprehensive course.
What is Balance?
Balance is the ability to maintain the body’s center of gravity over the base of support in a given sensory environment. We need to maintain our center of gravity, which is a point right about at L2, a little bit anterior to L2. Our base of support is the area between our legs that we’re standing on or between an assistive device, whatever is in contact with the ground. What’s important is this given sensory environment. Is it an uneven environment? Is there a lot of busy visual activity going on? But we have to maintain our balance, maintain the center of gravity over the base of support within whatever is going on.
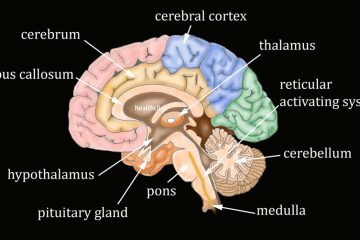
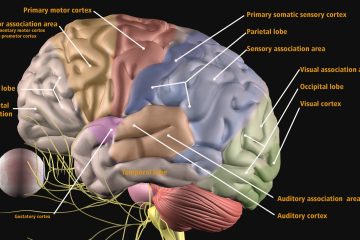
Contributors to Balance Dysfunction
A variety of factors can contribute to postural control and balance dysfunction; some include:
Motor contributors:
- decreased range of motion
- strength deficits
- motor control issues
- posture imbalance
Neurologic contributors:
- problems with reflexes
- radicular pain
- spasticity
- altered sensation
Sensory contributors:
- inability to use visual stimuli
- vestibular dysfunction
- inability to use somatosensory information for balance.
These factors can cause problems with any aspect of postural control and balance dysfunction.
Example of a Technique for Balance Retraining and Fall Prevention
Balance Training in Sitting
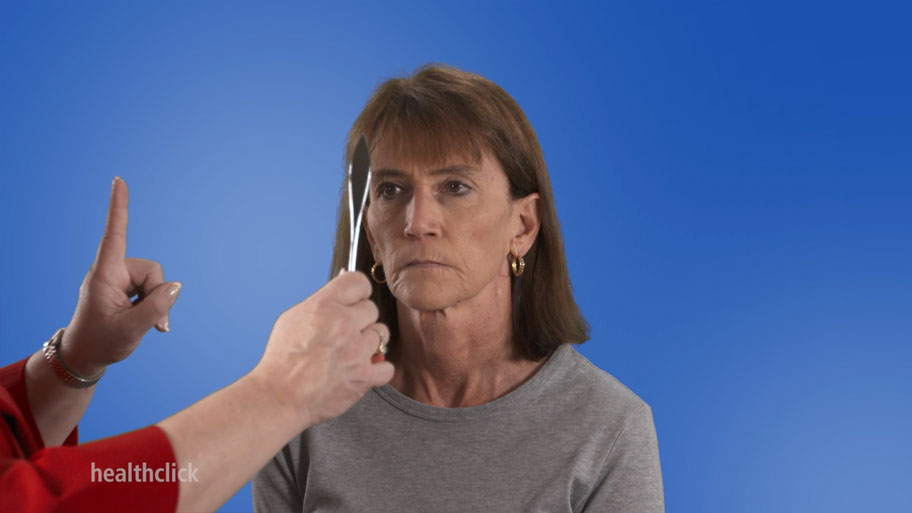
In doing balance training, we want to start with someone sitting if they’re having difficulty in sitting. This is for patients who have had a stroke with hemiparesis that may have trouble finding midline and moving out of it. It may be for people with Parkinson’s disease, M.S., or TBI. It may even be for people who’ve had problems with their lumbar spine that really don’t know where they are in space, and you can start working on this in sitting. You can do it on a firm surface, or you can do it on foam to challenge them.
Find Midline – Balance and Fall Prevention Continuing Education Course
What I do first is have them find midline. So, of course, she’s in nice midline, but if she was off to the side and sitting like this, then I would have her find midline and hold it. I can also do some perturbations to make her keep that position there. I can do some PNF techniques. I can also add in some upper extremity movements. So all those things can find the center. Remember, if someone’s not finding center, especially if they’ve had a stroke, often it’s a sensory issue. They’re not feeling that side and maybe pushing too much to one side to get sensory information. You may have to do other sensory techniques to try and get that even, so it may be doing as much as stimulating the sensory system on that side.
Falls are a threat to the health of older adults and can reduce their ability to remain independent.
https://www.cdc.gov/falls/index.html
Leaning on One Side
The next thing we’re going to do is I want her to lean to one side, so lean over as far as she can go and then come back up and find midline. I don’t want her overshooting or undershooting; I want this nice and smooth. I can use this as an evaluation as well as for treatment. And then I’m going to have her do it to the other side and come back up. I’m not over there to guard. All of these can be used in sitting to start.
Learn More!
For a comprehensive approach for PT courses on balance and fall prevention, go to www.healthclick.com and utilize the resources provided in the Balance and Falls Series of comprehensive courses within the All-Access Healthclick Subscription. Some of the courses in this series are:
Evidence Based Outcome Tools for Treating Balance Dysfunction
Balance and Falls in the Elderly Population
Treatment Approaches for the Neurological Progression of Multiple Sclerosis and Parkinsons’s Disease
Utilizing Pilates to Enhance Outcomes
Get Unlimited Access to all our Online Courses
- 12 months of unlimited access to the healthclick video course library with annual renewal.
- More than 300 hours of online video courses designed for Physical therapists, Occupational Therapists and Assistants.
- Access to future courses and content.
- Start, stop and resume, right where you left off in a course.
- Real patient interviews.
- Medical expert contributors.
- 3D anatomy and medical illustrations.
- Easy to use learning system for fast access to your courses.
- Award winning content.
- Top instructors teaching evidence based skills and techniques.
References
Wrisley, Diane M., et al. “Reliability, internal consistency, and validity of data obtained with the functional gait assessment.” Physical therapy 84.10 (2004): 906-918.
Whitney, Susan L., et al. “Clinical measurement of sit-to-stand performance in people with balance disorders: validity of data for the Five-Times-Sit-to-Stand Test.” Physical therapy 85.10 (2005): 1034-1045.
Avers, Dale. “The Value of Geriatric Physical Therapy: Excerpts from ‘We Can Do Better’: 2020 Carole B. Lewis Distinguished Lecture: Address to the APTA Geriatrics Membership at the Combined Sections Meeting, Denver, CO, February 13, 2020.” Journal of Geriatric Physical Therapy 43.3 (2020): 115-119.
Vincenzo, Jennifer L., et al. “Physical Therapists and Physical Therapist Assistants’ Knowledge and Use of the STEADI for Falls Risk Screening of Older Adults in Physical Therapy Practice in the United States.” International journal of environmental research and public health 19.3 (2022): 1354.
CDC.gov/falls/facts
The information in this Blog is intended for medical professionals only.