We must realize that while we’re looking at the shoulder and elbow, the shoulder and elbow are not the only pieces of the puzzle, especially when it comes to that throwing athlete. So we have to make sure that we’re looking at our spine, our core, our legs, our feet, our balance, and how we move, and all of those have to be in the comprehensive evaluation for that throwing athlete. The throwing-shoulder continuing education course focuses on manual therapy to optimize throwing mechanics and injury prevention in the Throwing Athlete, and is a comprehensive course on returning the athlete back to their sport.
What is the Role of Manual Therapy to Optimize Throwing Mechanics
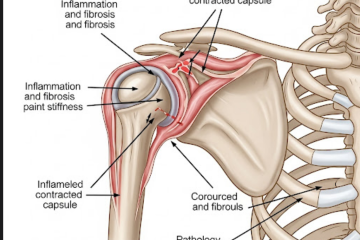
Let’s start talking about manual therapy for the shoulder and manual therapy in general. If we look at the research for manual therapy, we know it’s a little spotty. We know the changes we can make are very short-term if any. So the big thing with knowing that is that we have to take that little bit that we know, take our clinical decision-making, and decide what we need to do for our patient.
Appropriate Timing for Manual Therapy to Optimize Throwing Mechanics
I use a lot of manual therapy, especially at the beginning of our treatments. This is where you get to be hands-on with your patient and get to know them. Even though I’m not a dad, I tell many bad dad jokes, but it keeps them entertained and helps us gain that trust. It also gives me a hands-on feel of what that shoulder or what that elbow looks like and feels like. I will use both joint mobilizations and soft tissue work to help get me a better idea of what they’re feeling but also help with getting some of that mobility and motion back and decreasing pain.
Manual Therapy Research
Looking at the research, we know that our gains are very short-term and limited, so how a manual therapy treatment should always go is first, you’re going to assess your tissue. You’re going to look to see what range of motion am I looking to improve? Or what pain am I looking to decrease? Or what movement are they looking to make better? From there, you perform your manual therapy treatment. So if you’re doing joint mobilizations, you do that according to your treatment prescription. If you’re into soft tissue mobilization, you do that according to what you want to do as far as lengthening, treating, and decreasing the muscle’s sensitivity. From there, you have to make sure you take a reassessment because that is the biggest component. We have to make sure we’re making a change, so if we’re just putting our hands on somebody to put our hands on somebody, that’s very nice, but we have to make sure that we’re doing something that is helping our patients.
“The results of this study indicate the application of MET to the horizontal abductors provides acute improvements to GH horizontal adduction ROM in high school baseball and softball players, while joint mobilizations provide no improvements.“
NIH article
Re-Assessment
So now we’re taking that reassessment. Did we gain range of motion? Did we gain strength? Did we gain neuromuscular help? Did we decrease their pain? Then, if we did make gains, we have to do something to keep it. So the biggest mistake I see with many new grads–and let’s be honest, I made to start–is you stretch them. You do manual therapy, and great, I’ve made gains. Look at this range of motion that’s improved. You let him go home; good for me. You pat yourself on the back. Look at what I’m doing for this patient. They come back, and you’re like, “Oh, your range of motion. Your pain is back. Well, let’s do manual therapy again.” Again, now you’re in this cycle. You’re not doing anything to change that, so that’s where your therapeutic exercises become important.
Strengthening
You need to make sure you’re strengthening that end range. You need to make sure you’re doing something stretching-wise to keep that range or that pain down. We can’t get into this cycle as a profession of you come in, you do manual therapy, and you say hasta luego. So the biggest thing I’ll have is when patients come in, like, “Well, my doctor only wants you to do manual therapy.” Nope, sorry. I’m not a manual therapist. I’m a physical therapist. Manual therapy is a tool that I have, and it’s a tool that I use. I think it’s a great tool to have, but you have to make sure you’re doing something for that patient on the back end because otherwise, they’re just going to be in the cycle. You’re going to keep seeing them, and trust me; I’m a person that people don’t want to see for a long time.
If you would like a learn more about how to use manual therapy to optimize throwing mechanics sign up for the throwing continuing education course Injury Prevention and Optimal Mechanics in the Throwing Athlete. This is one course in the Healthclick All Access Online Series in our All Access Annual Subscription that contains various upper extremity orthopedic courses to Improve function. Check out some other courses within the orthopedic series:
Foundation Exercises for the Shoulder
Clinical Examination and Treatment of the Cervical and Thoracic Spine
References
Plummer HA, Plosser SM, Diaz PR, Lobb NJ, Michener LA. Effectiveness of a Shoulder Exercise Program in Division I Collegiate Baseball Players During the Fall Season. Int J Sports Phys Ther. 2022 Feb 1;17(2):247-258. doi: 10.26603/001c.31638. PMID: 35136694; PMCID: PMC8805093.
Reed ML, Begalle RL, Laudner KG. ACUTE EFFECTS OF MUSCLE ENERGY TECHNIQUE AND JOINT MOBILIZATION ON SHOULDER TIGHTNESS IN YOUTH THROWING ATHLETES: A RANDOMIZED CONTROLLED TRIAL. Int J Sports Phys Ther. 2018 Dec;13(6):1024-1031. PMID: 30534468; PMCID: PMC6253760.
Saper, Michael G., et al. “Epidemiology of shoulder and elbow injuries among United States high school baseball players: school years 2005-2006 through 2014-2015.” The American journal of sports medicine 46.1 (2018): 37-43.
Wright, Alexis A., et al. “Exercise prescription for overhead athletes with shoulder pathology: a systematic review with best evidence synthesis.” British journal of sports medicine 52.4 (2018): 231-237.