Stroke: Achieving Functional Movement in the Home Bound Patient
Learn something now! - Watch the Online CEU Course Trailer
All Access Online CEU for PT, PTA and OT for $189
BEST VALUE - Includes this course and all our online courses
Subscribe Todaytheaters Purchase Now, Instant Online Course Access
Stroke: Achieving Functional Movement in the Home Bound Patient
$160.00
- CE Hours: 8.5 hrs, .85 CEU
- Delivered: Online
- Instant Online Access, PDF Manual for Download, 365 days of access, Mobile Ready
- No auto-renewal for this option
All Access Online CEU for PT, PTA and OT
$189
All Access Online CEU for PT, PTA and OT Subscription
1 Year Access with Annual Renewal
State specific course completion certificates.
Chat support
Prices are in US dollars- 12 months of access to all online ceu courses, course tests and state approval certificates.
- Meet all your CE requirements. Pre-approved for PT, PTAs in AK, AL, AZ, CA, CO, CT, DC, DE, GA, HI, IA, ID, IL, IN, KS, MA, ME, MI, MO, MS, MT, NC, ND, NE, NH, NM, NV, NY, OR, PA, RI, SC, SD, TN, TX, UT, VA, VT, WA, WI, and WY.
- AOTA approved.
- Designed for Physical Therapists, Occupational Therapists, Athletic Trainers and Assistants.
- Access to future courses and content.
- Start, stop and resume, right where you left off in a course.
- Real patient interviews.
- Medical expert contributors.
- 3D anatomy and medical illustrations.
- Easy to use learning system for fast access to your courses.
- Award winning content.
- Top instructors teaching evidence based skills and techniques.
Why should a physical therapist, occupational therapist or athletic trainer take this stroke continuing education course?
Transitional rehabilitation parameters and guidelines are continually changing in today’s healthcare environment. More and more people opt to receive care as a home care patient during the pandemic and COVID-19. Managing a complex senior patient for residential care can differ between a patient transitioning to an assisted living facility or functioning independently in their home.
This stroke rehab course will prepare you to enter the home environment with a toolbox of evaluation and treatment techniques to assist the client in their individualized situation.
Rehab clinical tools instructed in this stroke rehab CE course to enhance your functional outcomes.
- Specific functional assessment tools to utilize in a variety of home care situations
- Developing the best treatment plan for the specific patient’s needs
- Principles and philosophy of PNF and their application to the stroke patient in the home care setting
Specific instruction that will enhance your understanding and ability to deliver better patient care.
- Therapeutic evaluation and treatment techniques as applied to two case studies with a diagnosis of s/p CVA
- Establishing baselines and gathering critical information for successful treatment in the home care setting
- Utilizing PNF techniques to progress function from the very low base level of dependent bed mobility to a higher level of function, such as gait
Features unique to this stroke rehabilitation continuing education course
- Exercises without the use of gym equipment to promote specific function
- Step-by-step case studies to assist the clinician with developing practical functional objectives
Professional Accreditation
This is an intermediate level course applicable for PT, PTA, OT, AT. Physical Therapy Accreditation: For specific state information use the accreditation verification menu and select your state of license. AOTA: provider #4487, Occupational therapy professional development activity: Foundation Knowledge: human body, development, and behavior. Athletic Trainers: BOC provider #P2047, category A. This course has not been submitted for Evidence-Based BOC approval.
fact_check Accreditation Verification
Online CEU Course for PT, PTA, OT State Accreditation
Course Objectives

Upon successful completion of this course the participant will be able to:
- Identify the key areas that need to be tested to establish a baseline of measures.
- Identify red flags and priorities for Stroke treatment.
- Identify the appropriate cognitive and functional evidence-based assessment tools to utilize when establishing baselines and progressions of care to reach targeted goals.
- Discuss the benefits to utilizing progressive developmental sequencing to optimize coordinated functional movement.
- Utilize evidence-based tools to evaluate deficits in mobility and/or stability in the complex geriatric patient.
- Develop strategies for reducing re-hospitalization rates.
- Prioritize impairments when developing comprehensive treatment programs for the geriatric patients with neurological and/or orthopedic problems.
- Analyze abnormalities in the components involved with functional movements and prioritize a treatment approach to improve an individual’s functional patterns of movement.
- Perform PNF techniques to improve functional mobility.
- Describe the initiation of movement (stability to mobility and coordination) when utilizing developments sequencing to enhance functional motion.
- Identify techniques to incorporate into the program for fall intervention and prevention.
- Incorporate specific exercises with and without equipment into a comprehensive program to improve functional mobility.
- Discuss how to develop a comprehensive rehab program for a variety of diagnoses in the home care environment.
Learn From the Expert - Suzanne White, PT

Suzanne White, PT, has over 30 years of experience as a physical therapist. She graduated from California State University Northridge. Her credentials include extensive experience in acute rehabilitation, inpatient rehabilitation, outpatient orthopedics, outpatient Neurorehabilitation and home health PT. She has been internationally recognized as a PNF advanced instructor. Suzanne has taught short term and long term courses in the United States as well as internationally in South Korea and Germany. Suzanne was on staff at Kaiser Foundation Rehabilitation Hospital from 1987-2000, where she was an advanced international instructor in the PNF residency program. She has completed numerous long-term manual therapy courses including the Folsom yearlong manual therapy course utilizing Maitland and Kaltenborn approach. She has been working in her own private Home Health practice for over 16 years. Working primarily with the complex geriatric patient, getting them back to living a more functional life and integrating the patient’s hobbies into her treatment plan.
Establish a Baseline

- Systematically review of all of your Geriatric Patients systems
- How is their cardiovascular system?
- Do they have congestive heart failure?
- Do they have chronic obstructive pulmonary disease?
- Are they on blood thinners?
- Are they on beta blockers?
- Skin integrity
- Metabolic-Diabetic?
- Dehydration/malnutrition
- Eye/ear checks?
- Psychiatric Medication usage
- Bowel and bladder
- Urgent bladder
- Neurological issues
- Chemotherapy
- How fast did they move/walk prior to needing to see a therapist
- Know your patient’s strengths along with their limitations
Functional Objective Measurement and Assessment

- Timed Get up and Go
- Activities-Specific Balance Confidence Scale-ABC
- Test of Reaction Time
- Functional Mobility Test
- five time sit to stand
- Cognitive Screening Tool
- Balance and falls
Building a Treatment Philosophy

- PNF Proprioception Neuromuscular Facilitation:
- Dr. Kabat and Maggie Knott PT and the basic philosophy of treatment
- Learn to treat the patient as a whole mind, body, spirit and emotion
- Reinforcing what the patient can do well
- People did not move in straight planes
- Treatments are functional
- Using the developmental sequence
- Creating stability, mobility & coordination.
- Usimg Repetition to promote, retain motor learning, to develop strength and endurance.
Case Study Post CVA-Ambulatory
Patient with a diagnosis of CVA
- Patients physical presentation
- Patients physical presentation and balance deficits
- Discussion of functional measurement tools
- Precautions for this type of patient
- Learn to create priorities of treatment
- Treatment for back pain
- The treatment approach for the patients back pain
- Treatment for balance dysfunction
- Treatment exercises
- Quadruped for muscle elongation and back pain
- Address frozen shoulder
- Treatment in prone
- High level training
- Review of treatment and progression into a home exercise program
- Building the best treatment program for CVA
- Discharge evaluation and plan
Case Study The Post CVA-Non-Ambulatory

- Learn to evaluate patient history and level of function
- Functional objective measurement tests
- Precautions and treatment priorities
- Determining baseline measures
- Treatment Techniques to initiate rolling:
- Sidelying, PNF pelvic patterns, dynamic reversals
- Sidelying, PNF pelvic patterns, anterior elevation and posterior depression
- Sidelying, PNF pelvic patterns posterior depression of the pelvis
- From supine: PNF patterns-flexion
- From supine and back: PNF patterns-extension
- From supine and back: PNF patterns-approximation
- Treatment to initiate coming up on the elbow
- From side-lying: irradiation
- From side-lying:manual cues
- To hand from side-lying:functional movements, mobility exercises
- Learn treatments to initiate coming from side-lying to sitting
- Treatments to initiate coming from side-lying to sitting
- Enhance sitting stability
- Understand vitals relative to patients position
- Techniques to move patient from sit to stand
- Review protocol for an eight week period
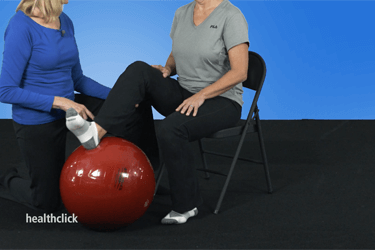
Exercises to Progress Functional Movement

- Develop a comprehensive floor exercise program
- In supine with therapy ball
- In supine with resistive band and prone on elbows
- In quadruped over ball
- To improve shoulder range of motion
- To progress from quadruped to kneeling and activities in kneeling
- Exercises in half kneeling
- Seated Exercises with resistance band and physioball
- Standing exercises working on balance activities
Course Test - Evaluate your knowledge
- Use the Healthclick proprietary online education system which provides the online student with:
- Worldwide access to high definition video, anatomical animations and images, and written information
- The highest quality film in the industry, you can see the difference!
- Stop and resume within a course, the Healthclick system will optimize your course based on your device, connection and remembers where you left off.
- Real-time course updates. We are always adding to each courses, updating content, adding animations, these are not static courses!
- Evaluate your knowledge with the course test on any device.
- Print your state course certificate for CE credit.
- Take the online test as many times as need in order to achieve a 70 % or greater score.